Long-Term Management of Transplants
Organ transplantation is the leading treatment for people with end stage disease of a particular organ, such as the liver or kidney. In the United States, the survival rate of patients who receive lung, kidney, heart, or liver transplants, along with the survival rate of the transplanted organ itself, is above 90%.1 This high survival rate depends in large part on the intensive long-term management of the complex and potentially life-threatening postoperative complications that transplant patients face. This article will focus on the long-term management of transplants for livers and kidneys, two of the most common organ transplants, as a way of exploring the careful and sometimes arduous management strategies required to navigate post-transplantation complications.
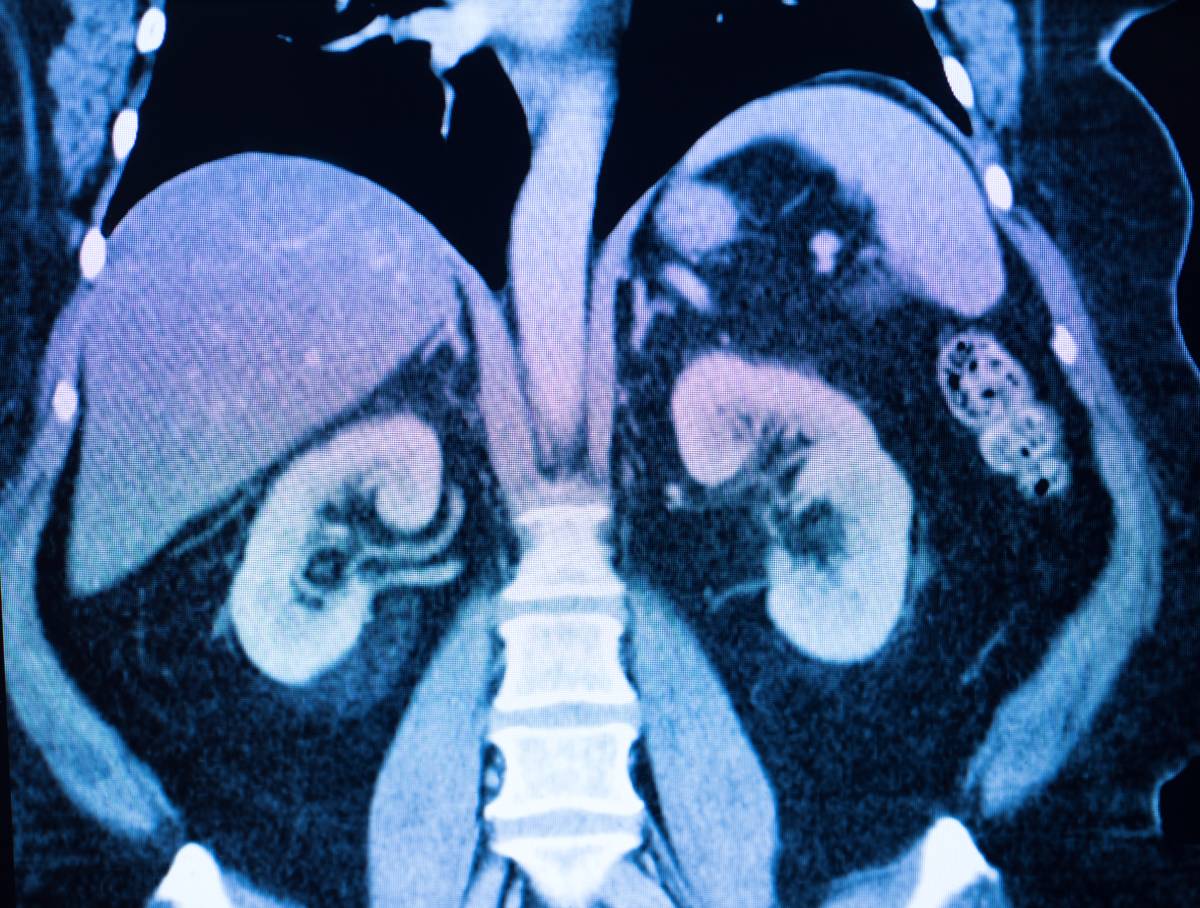
Kidney transplant patients are at a much higher risk of developing certain conditions as compared to the general population, even when the graft functions perfectly. For example, kidney transplant patients have a 3.5-5% chance of succumbing to cardiovascular disease, which is 50 times higher than the general population.2 Many graft recipients also suffer from hypertension, diabetes, and dyslipidemia (an abnormal amount of lipids in the blood), possibly on account of the immunosuppressive agents they receive before and after surgery, which are associated with these diseases.3 Other complications of a kidney transplant include anemia and the loss of bone, the latter of which can result in fractures.4
The abovementioned complications are not unique to transplant patients and can be treated in the same manner as they are in non-transplant patients, provided that care be taken to prevent exacerbating the unique complications faced by kidney transplant patients. These include graft dysfunction and infection. After ensuring that acute kidney rejection or injury has not occurred, physicians will then determine if the patient may have chronic allograft nephropathy, which is defined as graft dysfunction occurring 3 months or more after transplantation unrelated to infection or other diseases.4 This can be treated by limiting exposure to calcineurin inhibitor after surgery, an immunosuppressant commonly used for transplantation but one that can cause nephrotoxicity at higher exposures.
Liver transplants also have their own similar set of postoperative complications and management steps. Among the most common are hypertension, which occurs in 60-70% of patients after orthotopic liver transplant (substitution of the entire diseased liver with a healthy one), and diabetes, which has an incidence of 30-40%.5 Antihypertensive agents, such as dihydropyridine calcium channel blockers, which cause the widening of arteries, are recommended for postoperative hypertension, while management of postoperative diabetes is similar to that of diabetes in the general population: insulin is often required, and the use of corticosteroids may be withdrawn.5
Interestingly, chronic kidney disease is a complication in liver transplant patients. Defined as the presence of a reduced filtration rate for 3 months or more, chronic kidney disease occurs in liver transplant patients with increasing frequency in the years after surgery. Its etiology in the context of liver transplantation may involve hypertension, diabetes, and the use of calcineurin inhibitors.6 If diagnosed early, chronic kidney disease can be managed by either limiting CNI doses or introducing CNI-free regimens of immunosuppressive drugs.
References
1. Outcome Measures for Organ Transplantation | UC San Diego Health. UC Health – UC San Diego https://health.ucsd.edu/specialties/transplant/Pages/quality.aspx.
2. Ojo, A. O. Cardiovascular complications after renal transplantation and their prevention. Transplantation 82, 603–611 (2006), DOI: 10.1097/01.tp.0000235527.81917.fe
3. Kasiske, B. L. Ischemic heart disease after renal transplantation. Kidney Int. 61, 356–369 (2002), DOI: 10.1046/j.1523-1755.2002.00121.x
4. Schaefer, H. M. Long-Term Management of the Kidney Transplant Recipient. Blood Purif. 33, 205–211 (2012), DOI: 10.1159/000334158
5. Singh, S. & Watt, K. D. Long-term Medical Management of the Liver Transplant Recipient: What the Primary Care Physician Needs to Know. Mayo Clin. Proc. 87, 779–790 (2012), DOI: 10.1016/j.mayocp.2012.02.021
6. O’Riordan, A., Wong, V., McCormick, P. A., Hegarty, J. E. & Watson, A. J. Chronic kidney disease post-liver transplantation. Nephrol. Dial. Transplant. 21, 2630–2636 (2006), DOI: 10.1093/ndt/gfl247
